Hemorrhoids are also known as varicose veins. They comprise veins that are swollen and enlarged. These veins are divided into two types; external hemorrhoids, and internal hemorrhoids.
Contents
External hemorrhoids are more visible than internal hemorrhoids, appearing as protrusions or lumps all around the rectum. This form of hemorrhoids is prone to becoming painful, bloated, unpleasant, and agonizing.
Internal hemorrhoids are much more frequent than superficial hemorrhoids. Internal hemorrhoids have the tendency to affect anyone, but they aren't a bother until the capillaries in the rectum enlarge and the membrane starts to unravel.
Minimal oozing of blood is a frequent sign of internal hemorrhoid, and if the enlargement progresses, you might begin to understand several of the usual hemorrhoid symptoms. Inner hemorrhoids are commonly caused by congestion, but because there are very few neurons within this area of your anus, you may still not experience any discomfort.
Internal hemorrhoid epithelium can flow even outside the anus as ruptured hemorrhoids as time goes on. An experienced physician can tell whether you have an outer hemorrhoid or inside hemorrhoid that has distended. If you detect a little volume of blood on using a toilet roll or feel penile skin surrounding your rectum, you ought to see your specialist determine the cause and get assistance.
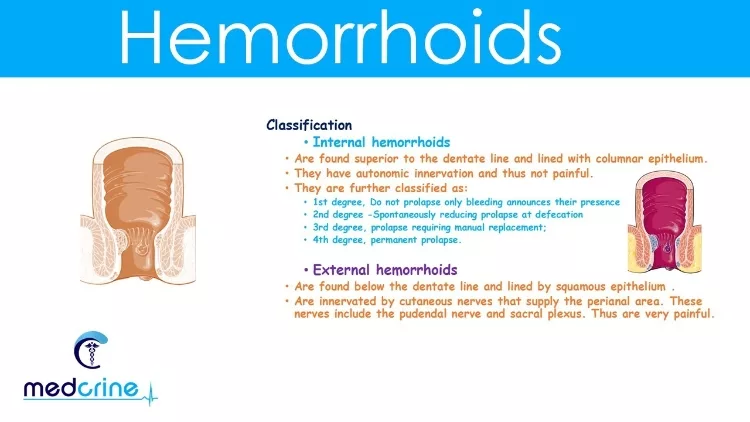
Above the dentate line (the irregular circle that is formed by the collision of anal valves), there is a hemorrhoidal venous plexus. On the lower side of the venous plexus, internal hemorrhoids are originated. It is surrounded and covered by mucosa.
Whereas, external hemorrhoids are distorted vesicles of the same venous plexus that, contrary to internal hemorrhoids being located inferior to the venous plexus, are present on the bottom line of the irregular anal valves circle. It is covered and surrounded by squamous epithelium.
To get a better insight into the difference between hemorrhoids, fissures, and fistulas, watch this short video:
A hemorrhoid grading plan is vital both for determining which therapies to utilize, as well as for comparing therapeutic efficacy. Hemorrhoids are categorized based on where they are positioned and how far they have prolapsed.
Internal hemorrhoids aren't all just the same, and they don't all create the very same issues. Internal hemorrhoids are classified into four severity levels by doctors, mentioned below:
First-degree hemorrhoid originates when internal hemorrhoid oozes but stays within the colon. Although the rectal tissues leak, they would not fall.
Internal hemorrhoids can rupture, which means they expand beyond the rectum. A second-degree hemorrhoid is one in which distended hemorrhoid resolves and heals by shrinking on its own. When you push, the rectal valves leak through the anus, but they diminish on their own.
A distended third-degree hemorrhoid doesn't quite diminish by itself. Such hemorrhoids, otherwise, respond positively to physical compression and can be forced back inside the anus.
Internal hemorrhoids, according to the fourth-degree, are by far the most progressed and aggressive kind. These are irreversible distended hemorrhoids, suggesting they will stay distended regardless of the human reduction strategies.
The rupture is permanent and cannot be reduced. Fourth-degree hemorrhoids include intensely swollen glands, imprisoned internal hemorrhoids, and interned, stenotic hemorrhoids causing peripheral rectal membrane protrusion.
Hemorrhoids are most commonly manifested by mild internally oriented rectal bleeding concomitant with bathroom visits, which sufferers report as red drops into the toilet. Because hemorrhoidal mucosa has an immediate arterio-venous connection, the flow is usually bright crimson.
Whenever the blood loss is aberrant for hemorrhoids, if no reference of blood loss is visible on anal assessment, or when the person has major public health problem for colon carcinoma, positive urine tests blood or anemia should also not be directly linked to hemorrhoids before the bladder has been appropriately assessed.
Internal hemorrhoids are caused by enlarged and engorged capillaries in the anus. Internal hemorrhoids occur at the lowest portion of the rectum, but they're quite distant enough within that the patient might not even notice they're present. Although blood has been the most prevalent sign of internal hemorrhoids, a prolapsed hemorrhoid can cause a variety of other complaints. This usually occurs with a bowel movement, and the mucosa will usually return in by itself. In some situations, you may also need to re-insert the mucosa. The tissue will stay prolapsed in the event of fourth-degree hemorrhoids.
It's crucial to remember that colorectal cancer, as well as the type of hemorrhoids that is called internal hemorrhoids, both can cause bleeding. That's why, if you're having any rectal bleeding, you should visit a doctor immediately once, particularly if it's followed by several other suspicious indications.

Some of the many causes or reasons that lead to experiencing internal hemorrhoids are mentioned below:
Those suffering from internal piles have a variety of therapy choices. People are acquainted with several hemorrhoid procedures that seek to provide short help and treatment, stinging, or overall annoyance. Sitz baths, over-the-counter balms and serums, and perfect home treatments like shea butter and apple cider are examples of these techniques. Unfortunately, these treatments are only effective for external hemorrhoid symptoms and only give temporary relief. Internal hemorrhoids therapy must be targeted at permanently resolving the condition by eliminating the internal hemorrhoids. Some of these treatments include:
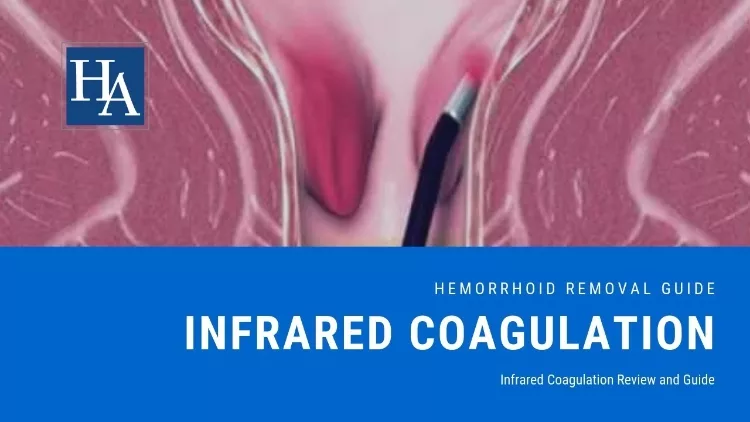
Infrared coagulation is a less intrusive alternative to surgery (IRC). A medical expert will shine infrared radiation on inner hemorrhoids, causing fibrosis to develop and blocking blood circulation to the blister. The epithelial tissue will come off after about a week, and minor hemorrhaging is probable.
Drawback:
There are recurring bleeding cases reported post-therapy that includes infrared coagulation.
Here is the video representation of this procedure:

Sclerotherapy is yet another less invasive therapeutic option. This treatment is known to certain individuals as a means to cure varicose veins. A medical practitioner will infuse a chemical substance into the rectum's enlarged veins, causing the veins to shrink and constrict. To properly resolve the problem, the technique may need to be done several times.
Drawback:
It is not much efficient when it comes to progressive, severe hemorrhoids. It is more effective on small blister-like hemorrhoids.
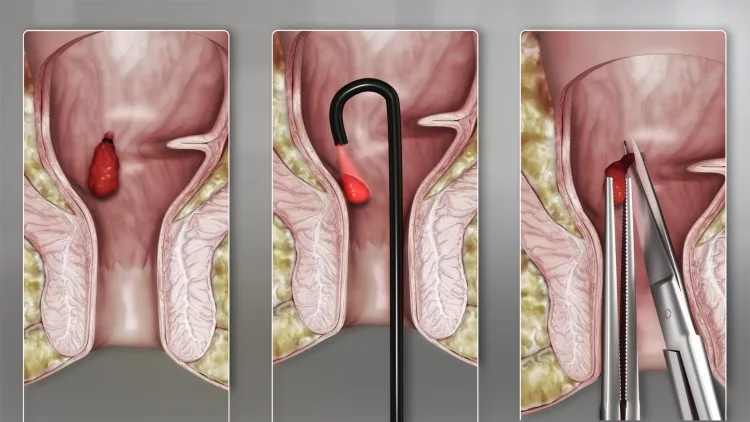
Internal hemorrhoids can be removed and prevented using banding, which is among the most effective methods. Endoscopy banding may appear to be a wider choice, but it is a time-consuming operation that necessitates pretreatment and anesthesia. The CRH O'Regan Method for hemorrhoid banding is a superior alternative to chemical hemorrhoid wrapping techniques. Tiny reusable legator forceps are used in a gentle aspiration rather than metal forceps to maintain the afflicted capillary in location. This approach does not involve any pretreatment or anesthesia, is painless, and should leave you feeling fine afterward.
Radiofrequency ablation (RFA) is a pretty new therapeutic option for hemorrhoids. The venous stasis mucosa is contacted by a ball wire linked to a dipole generator, which causes the encountering tissue to coalesce and vaporize. The circulatory elements of hemorrhoids are decreased with such a technique, and the venous stasis mass is attached to the deeper tissues by scarring. RFA, like sclerotherapy, can indeed be done as an emergency visit using an anoscope. Acute urine incontinence, internal bleeding, and perianal thromboembolism are among the consequences.
Drawback:
Despite the fact that RFA is a painless technique, it is linked to a greater incidence of repeated hemorrhage and prolapse.
Cryotherapy uses a frozen cryogenic cryoprobe to remove excess hemorrhoid tissue. Because sensitive neurons are damaged at such low temperatures, it is said to produce less discomfort. However, it was linked to protracted discomfort, foul-smelling waste, and a high risk of persisting venous stasis mass in numerous human researches. As a result, it is rarely utilized.
When compared to conventional techniques, percutaneous hemorrhoidectomy is perhaps the most successful therapy for hemorrhoids, with the fewest risk of progression. Blades, laser surgery, or a venous device like Ligasure or a Harmonic scalpel can all be used. As a mobile operation, percutaneous hemorrhoidectomy could be conducted comfortably under perianal anesthetic infusion. The difficulty of non-operative treatment, acute complex hemorrhoids such as constriction or clotting, patient choice, and concurrent anorectal diseases such as anal fissure that necessitate surgery are all reasons for hemorrhoidectomy, including third and fourth-degree conditions.
Drawback:
Postpartum discomfort is a significant disadvantage of hemorrhoidectomy. In comparison to forceps or electrocautery hemorrhoidectomy, Ligasure hemorrhoidectomy is said to result in reduced postoperative discomfort, shorter hospitalization, quicker skin health, and faster recovery.
For a better understanding of this procedure, watch this video below:
In this guide, we tried to cover all the possible aspects of internal hemorrhoids that might help you in inspecting your condition. From indications to the treatments, we mentioned it all. However, don't forget to seek medical assistance or seat cushions in case of any health inconvenience.
If you found this guide helpful, don't forget to share it with your friends and family who might need some medical guidance.
Thank you! Stay healthy!
 |
 |
 |
 |